What is a Chronic Wound?
In brief, a chronic wound is a wound that has not healed for more than 4-6 weeks. A simple cut or small wound, if there are underlying health issues, can remain open for a longer period than usual and may turn into a chronic wound. Underlying significant causes, such as diabetes, circulatory disorders, or prolonged immobility (pressure sores due to bed rest), often play a role in the formation of chronic wounds. These wounds are mostly seen on the legs, especially on the feet and lower legs. Chronic wounds are not just open wounds on the skin that do not heal over time, but also a serious health issue that significantly lowers the person’s quality of life, increases the risk of infection, and even leads to limb loss.
In this article, we will discuss the most common causes of chronic wounds in a simple and understandable manner. We will examine various causes, ranging from diabetic wounds to ulcers caused by circulatory disorders and pressure (bed) sores. Additionally, we will touch on advanced methods used in chronic wound care and treatment, including regenerative approaches such as exosome therapy, which has shown promising results in recent years.
What Are the Causes of Chronic Wounds?
In order for a chronic wound to develop, there is usually an underlying condition or a factor that complicates the healing process. Below are the main causes of chronic wound formation, listed by headings:

Circulatory Disorders (Arterial Issues)
Problems in blood circulation are one of the most common causes of chronic wounds. Arteries carry oxygen and nutrients to tissues; when there is narrowing or blockage in the arteries, sufficient blood cannot reach the wound, and healing slows down. An example of this condition is peripheral artery disease (blockage of the leg arteries). Particularly, reduced blood flow to the legs makes it difficult for even small wounds on the feet or legs to heal. As a result, these wounds, which cannot be nourished by adequate blood supply, can become chronic. Chronic wounds due to arterial blockage can lead to severe consequences, including limb loss in advanced cases. Therefore, it is crucial to control risk factors such as smoking, high cholesterol, and arteriosclerosis that lead to arterial blockages.
Venous Disorders (Varicose Veins and Venous Ulcers)
Veins are blood vessels that carry blood from the legs back to the heart. When the valve in the veins weakens or varicose veins develop, blood pools in the legs and pressure increases. In this situation, the skin and tissue cannot receive enough oxygen. Especially, even a simple injury on the ankle or lower leg in these unfavorable circulation conditions struggles to heal and can turn into a chronic wound. Venous ulcers, commonly known as “open leg wounds,” occur through this mechanism. Wounds caused by progressing varicose vein disease are usually difficult to treat and should be evaluated by a specialist doctor, with appropriate dressings and, if necessary, compression therapy (such as compression stockings). In venous wounds, treating the underlying varicose or venous insufficiency problem (such as correcting varicose veins through surgical or interventional methods) is critical for healing.
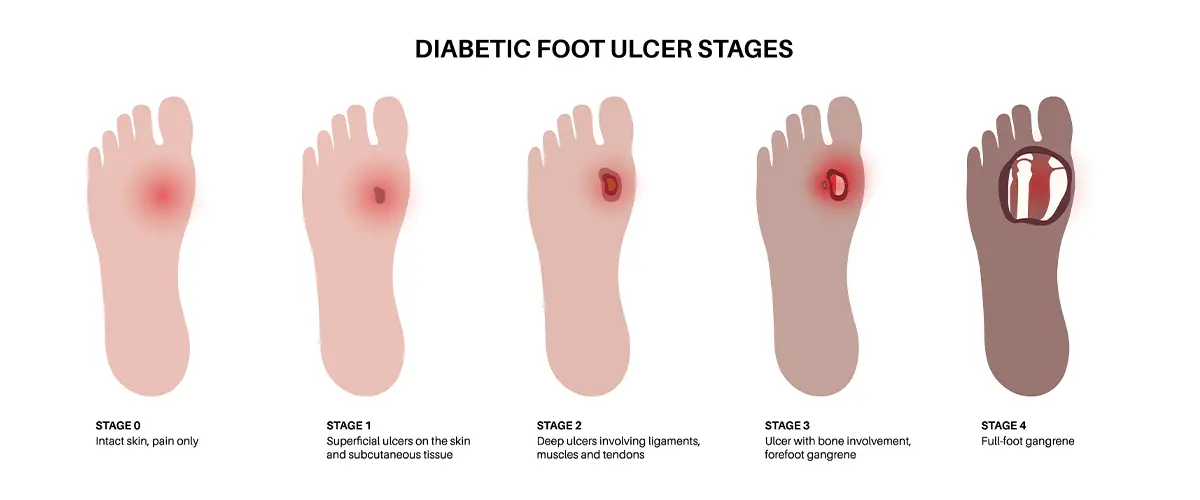
Diabetes (Diabetes Mellitus) and Diabetic Foot Ulcers
Diabetes is one of the first causes that come to mind when thinking about chronic wounds. Diabetes affects both the blood vessels and nerves, making it harder for wounds to heal. In people with long-term diabetes, the arteries in the legs may narrow, and blood flow in small capillaries may be impaired. Additionally, due to nerve damage (diabetic neuropathy), patients may not feel small wounds like cuts or blisters on their feet. For example, a blister or corn caused by tight shoes in a diabetic patient may grow unnoticed and become infected. The tissue is deprived of nutrients due to inadequate blood circulation, and if an infection develops, the wound can quickly deepen. In this “diabetic foot” condition, even a small redness can turn into a serious wound; if not treated promptly, severe infections that may lead to amputation (limb loss) can develop. To prevent diabetic wounds, it is essential to keep blood sugar levels under control, perform daily foot examinations, use appropriate footwear, and pay attention to skin care.

Weak Immune System and Other Health Issues
A weak immune system is also a significant factor in slow wound healing. Advanced age, poor nutrition, serious illnesses like cancer, or the use of certain medications such as corticosteroids can weaken the immune system. In individuals with weakened immunity, the body struggles to repair wounds, fighting infections becomes more difficult, and healing times are prolonged. For example, simple wounds in individuals undergoing cancer treatment or those with chronic diseases may take longer to heal than usual. Additionally, factors that affect overall health, such as obesity (excess weight) and smoking, increase the risk of chronic wounds. Obesity increases the load on the wound and the oxygen demand in the tissue, while also impairing blood circulation; smoking narrows the blood vessels, reducing oxygenation, and disrupts collagen production, which is essential for wound healing. Therefore, in patients with chronic wounds, regulating nutrition, providing vitamin/protein support when necessary, and quitting harmful habits are crucial steps to accelerate healing.

Prolonged Pressure and Bed (Pressure) Sores
Pressure sores, commonly seen in patients with limited mobility or bedridden individuals, are another significant cause of chronic wounds. Continuous lying down or sitting in a wheelchair applies pressure from body weight to certain areas of the skin for extended periods. These pressure points are most commonly found on areas like the tailbone, hips, heels, and back. This pressure reduces blood flow to the skin, causing tissue damage. Initially, pressure sores appear as redness and discoloration of the skin, but if no precautions are taken, they can deepen into open wounds. If these wounds become infected, their treatment becomes even more difficult. The most important step in preventing and treating pressure sores is relieving or reducing pressure. To achieve this, the patient’s position should be changed frequently, special pressure-relieving beds and cushions should be used, and the skin should be kept clean and dry. If bedsores have already developed, appropriate wound care (such as cleaning dead tissue, infection control, and using moist wound dressings) should be performed by evaluating the wound stage. Remember, when you notice even a small redness in an immobile patient, reporting it to the healthcare team immediately can help prevent deeper wounds from developing in the future.
Severe Injuries, Burns, and Surgical Wound Complications
Sometimes, the direct cause of chronic wound formation is the trauma itself. Severe physical trauma (such as falls, collisions, or traffic accidents) or large surface area burns can overwhelm the body’s repair capacity. In large and deep injuries or high-degree burns, tissue struggles to regenerate, and wounds that would normally take weeks to heal can become chronic. For example, a third-degree burn may heal very slowly due to the risk of infection and significant tissue loss. Similarly, surgical wounds that do not heal properly, or those that become infected due to stitches or the patient’s underlying conditions, can also transform into chronic wounds that do not close. In these cases, plastic surgery interventions, skin grafts (patch applications), or vacuum-assisted devices may be needed to close the wound. In summary, in trauma and burn-related chronic wounds, the primary issue is the size and depth of the wound; the care of these wounds requires just as much attention and expertise as chronic wounds caused by underlying diseases.
The image above compares the initial chronic wound on the foot of a diabetic patient (on the left) with a healthy foot (on the right). In a patient with reduced nerve sensation due to diabetes, even a small wound can go unnoticed and progress into a serious chronic wound. Therefore, early intervention in diabetic foot ulcers is crucial.
Chronic Wound Care and Treatment Methods
To treat a chronic wound, it is essential to first eliminate or control the underlying cause. For example, if a leg wound is caused by arterial blockage, improving circulation (possibly through surgery), lowering blood sugar in diabetic wounds, or reducing pressure in pressure sores by repositioning the patient, are the first steps. Local treatments without addressing the underlying cause will be insufficient.
Local wound care forms the foundation of every chronic wound treatment. In this process, the wound is evaluated for signs of infection and cleaned appropriately. If dead tissue is present, it is removed through a procedure called debridement, using surgical instruments or special solutions, to encourage the healing of healthy tissue. In the presence of infection, antibiotics and antiseptic solutions are used as per the doctor’s recommendation. Modern wound dressings (hydrogels, foams, alginates, etc.) are used to maintain the proper moisture balance. The goal is to ensure that the wound is neither too dry, which may cause scabbing, nor too wet, which can lead to skin maceration. Every chronic wound is unique; therefore, the treatment plan, including dressing frequency and the materials used, should be determined by healthcare professionals based on the wound’s characteristics and the patient’s condition.
Additionally, supporting the patient’s overall condition is crucial. Wound healing involves the entire body. Adequate protein and vitamin intake should be ensured (and a dietitian’s support should be sought if necessary), and chronic diseases (such as diabetes, thyroid disorders, anemia) should be treated and kept under control. If the patient smokes, they should be supported in quitting, as toxins in cigarette smoke damage blood vessels and hinder oxygen transport, slowing down healing. To improve circulation, exercises or physical therapy methods can be implemented with the doctor’s recommendation. When all these general measures are combined with local wound care, the chances of healing a chronic wound significantly increase.
Wound, Diabetic Foot, Regenerative Medicine - Exosome FAQs
Why Do Chronic Wounds Heal Slowly?
Diabetes, circulatory disorders, infections, and improper dressing application all contribute to the difficulty of chronic wound healing. A multidisciplinary approach is required.
What is Regenerative Medicine?
Regenerative medicine includes treatments that encourage damaged tissues to repair themselves. Techniques such as PRP, stem cells, exosomes, and laser are part of this field.
What is PRP, and in which wounds is it used?
PRP (Platelet Rich Plasma) is used in wounds and surgical wounds, where healing cells derived from the patient’s own blood are applied to the wound.
What are exosomes and what are they used for?
Exosomes are microscopic structures that enable communication between cells. They support tissue regeneration through the growth factors they contain and are used particularly in wound healing and skin rejuvenation.
In which conditions is exosome therapy used?
Exosome therapy can be used in slowly healing chronic wounds, diabetic foot, vasculitis-related skin disorders, and aesthetic regeneration areas.
What is the difference between exosome and PRP?
While PRP is obtained from the patient’s own blood, exosomes are biological carriers obtained from cell production systems. Exosomes carry biological signals in a purer form and higher concentration.
How often should wound care be done?
Wound care should be planned based on the type of wound, its depth, and infection status, with care being performed either daily or more frequently as needed. It should be done under the supervision of a doctor.
Which wounds are suitable for regenerative treatment?
Non-healing venous ulcers, diabetic wounds, pressure sores, and tissue loss related to trauma are candidates for regenerative treatment.
When is a non-healing wound at risk?
If a wound has not healed after 4 weeks, is infected, or has a foul odor or black discoloration, advanced treatment is required. The wound should be evaluated by a specialist or a wound center.
Is medication required in chronic wound treatment?
Yes, especially in infected wounds, antibiotics may be used. In non-infected chronic wounds, medications that increase blood flow and support tissue regeneration may be prescribed. Additionally, topical agents that reduce inflammation in the wound area are also preferred.
Which medications are used to reduce pain and inflammation in venous ulcers?
NSAIDs (such as ibuprofen, diclofenac) are used to reduce pain.
Short-term antibiotic treatment when necessary.
Topical enzymes and healing agents (such as hyaluronic acid, honey-based creams).
Should be combined with bandaging.
What should I eat to speed up chronic wound healing?
Protein: Eggs, yogurt, meat, fish (for tissue repair)
Vitamin C: Citrus fruits, peppers (increases collagen production)
Zinc: Pumpkin seeds, red meat
Iron: Dark green leafy vegetables, dry legumes
Vitamins A and E: Carrots, almonds, olive oil