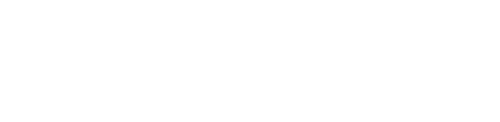
Arteries are the blood vessels that carry blood from the heart to the organs of the body. Diseases affecting these vessels can lead to serious health problems by preventing organs from receiving enough blood and oxygen. Under the title of arterial diseases, the five most common arterial conditions will be discussed: atherosclerosis (hardening of the arteries), arterial occlusion (blockage), aneurysm (vessel ballooning), peripheral artery disease, and carotid artery disease (disease of the carotid artery). Each disease is explained in simple language that patients can easily understand, including what it is, its symptoms, who is most at risk, diagnostic methods, and treatment options. In this way, concepts such as “arterial blockage” and “atherosclerosis” will become more comprehensible and contribute to increased health awareness.
Atherosclerosis (Arteriosclerosis)
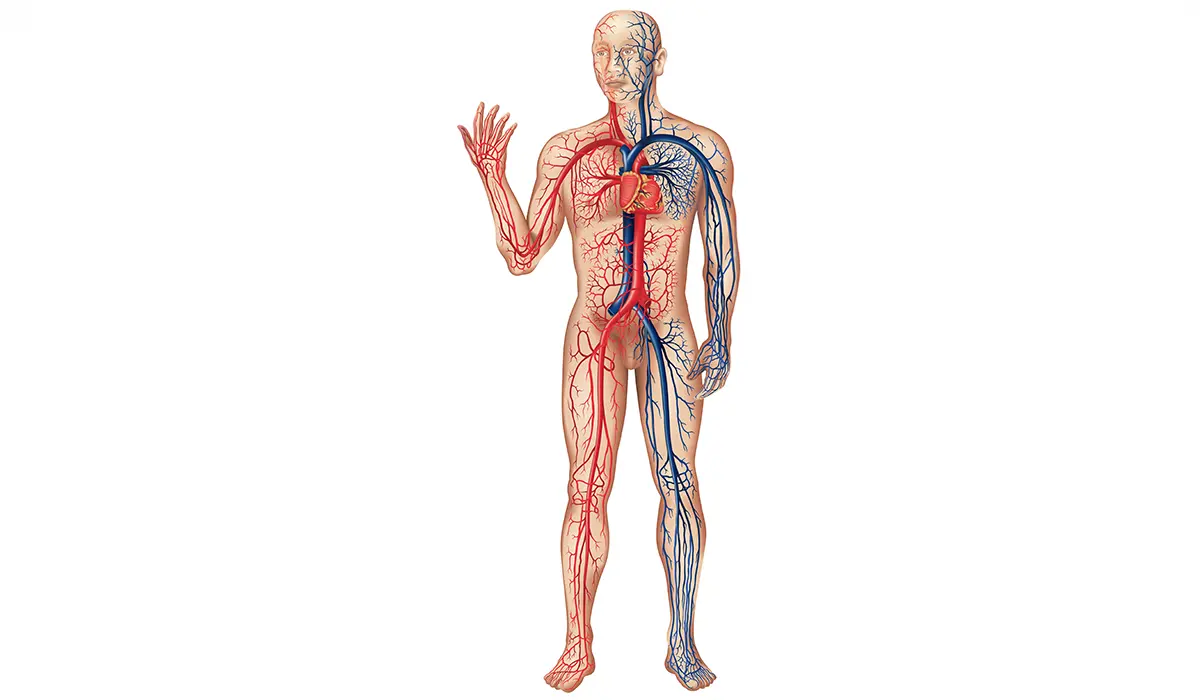
Atherosclerosis is the loss of elasticity and hardening of the arteries due to the buildup of cholesterol- and calcium-containing plaques on the arterial walls. This condition narrows the inner diameter of the arteries and reduces blood flow. Atherosclerosis typically develops slowly over the years and can affect all arteries in the body. It most often appears in the coronary arteries that supply the heart, increasing the risk of heart attack. It is also a very common vascular disease that can lead to serious problems such as stroke and peripheral artery disease. Atherosclerosis is more frequently seen in older adults, men, and individuals with risk factors such as high cholesterol, high blood pressure, diabetes, and smoking.
Symptoms
Atherosclerosis usually does not cause symptoms; however, complaints may arise depending on the organ damage it causes. The main symptoms include:
Chest pain (angina): Burning or pressure-like pain in the center of the chest that occurs with exertion and resolves with rest (if the heart arteries are affected). In advanced stages, chest pain may even occur at rest, or a heart attack can develop directly.
Leg pain: Cramping pain and fatigue in the calf muscles while walking (a sign of peripheral artery disease if the leg arteries are affected). This pain subsides with rest, but as arterial narrowing progresses, pain occurs over shorter distances.
Stroke symptoms: If there is significant narrowing of the brain arteries, signs of a transient ischemic attack or stroke may appear. For example, neurological symptoms such as numbness or weakness on one side of the body, speech disturbances, or vision loss may develop.
In many cases, atherosclerosis may not cause noticeable symptoms for a long time. Sometimes, the first sign can be a serious event like a heart attack or stroke.
Diagnosis
To diagnose atherosclerosis, a physical examination is performed and certain tests may be requested:
Blood tests: Measurement of cholesterol, triglycerides, and blood sugar levels (to assess important risk factors for atherosclerosis).
Heart tests: Examinations such as ECG (electrocardiogram), stress test, or cardiac ultrasound (ECHO) may be performed to evaluate the degree of involvement of the heart arteries.
Imaging: Color Doppler ultrasound can be used to visualize the condition of the arteries. For a definitive diagnosis, angiography (imaging of the arteries by injecting contrast dye) may be performed if necessary; for example, coronary angiography can be used to detect narrowing in the coronary arteries.
Treatment
Lifestyle changes: Quitting tobacco products, eating a healthy (low-fat and low-cholesterol) diet, reaching an ideal weight, and exercising regularly are essential steps. These changes can slow the progression of atherosclerosis.
Medication: If necessary, your doctor may prescribe cholesterol-lowering statins, antihypertensives, diabetes medications, or blood thinners to control high cholesterol and blood pressure. These medications help reduce plaque buildup and lower the risk of arterial blockage.
Angioplasty and stent: In advanced cases of arterial narrowing, interventional procedures may be required to open the artery. During angiography, a thin catheter is used to reach the blocked area, and balloon angioplasty can be performed; if needed, a stent (a small metal mesh) is placed to widen the narrowed artery. This method is frequently used to open blockages in heart arteries (e.g., coronary stent) or leg arteries.
Surgical treatment (bypass): In some widespread and advanced occlusive arterial diseases, surgical bypass surgery may be necessary. In this procedure, a healthy vessel (or synthetic graft) taken from another part of the body is used to create an alternative route beyond the blocked artery. Bypass surgery improves blood supply to the organ by directing blood flow past the obstruction.
Arterial Occlusion (Arterial Blockage)
Arterial occlusion is the partial or complete blockage of an artery due to a blood clot or atherosclerotic plaque, resulting in the interruption of blood flow. As a result of this blockage, the tissues supplied by the artery do not receive enough oxygen, and ischemia (lack of blood supply) develops. Arterial occlusions usually occur on the basis of atherosclerosis, when a clot forms on a narrowed plaque within the artery, or when a clot formed elsewhere suddenly travels (embolism) and lodges in a particular artery. Although it can occur in any artery in the body, in clinical practice, blockages of the heart (coronary arteries), legs, and neck (carotid arteries) are of the greatest significance. Severe arterial occlusions are medical emergencies that can lead to life-threatening complications such as heart attack, stroke, or loss of a limb.
Symptoms
Symptoms vary depending on the location of the blocked artery. The main symptoms include:
Blockage of a heart artery (coronary artery occlusion): Signs of a heart attack appear, such as severe chest pain, shortness of breath, heart palpitations, sweating, and nausea. This condition is usually caused by a clot forming on a plaque in the coronary arteries and requires emergency treatment.
Sudden blockage of a leg artery: There is a sudden onset of severe pain, coldness, paleness, and loss of strength in the affected leg; pulses in the foot or leg cannot be felt. If treatment is delayed, irreversible tissue damage may occur, and there is a risk of gangrene. This situation is usually caused by an embolism (a clot traveling from the heart to the leg artery) and is called acute limb ischemia.
Note: In case of sudden blockage of the brain arteries, stroke symptoms develop; these symptoms are explained in detail in the “Carotid Artery Disease” section.
Diagnosis
If arterial occlusion is suspected, blood circulation in the affected area is first evaluated:
Physical examination: Weakening or loss of pulses in the area supplied by the potentially blocked artery (such as in the legs or feet) is an important finding. The affected limb may also be cold and pale. In the case of a heart attack, a heart murmur or arrhythmia may be detected.
Imaging tests: The condition of the artery can be examined with Doppler ultrasound to identify areas where blood flow has slowed or stopped. For a definitive diagnosis, angiography is performed; in this procedure, contrast dye is injected into the relevant artery to clearly visualize the location and extent of the blockage. Coronary angiography is used for heart artery blockages, while peripheral angiography is used for blockages in the leg arteries.
Other tests: For heart attack diagnosis, ECG and blood tests for heart enzymes (such as troponin) are performed. In blockages of the legs or other regions, advanced imaging methods such as magnetic resonance angiography (MRA) or computed tomography angiography may be used when necessary.
Treatment
Emergency treatment: When arterial occlusion develops acutely (for example, during a sudden heart attack or blockage in a leg artery), the blocked artery must be opened as soon as possible. For this purpose, clot-dissolving drugs (thrombolytic therapy) can be administered intravenously in a hospital setting, or the clot can be removed by reaching the blocked artery with a catheter (embolectomy). In cases of heart artery blockages, the most common emergency treatment is balloon angioplasty and stent placement performed during angiography. In this way, the blockage in the heart artery can be opened within minutes, preventing damage to the heart muscle.
Long-term treatment: For a patient who has experienced arterial occlusion, it is essential to control the underlying risk factors to prevent recurrence. This includes cholesterol-lowering, blood pressure and diabetes-regulating treatments; in addition, blood thinners (anticoagulant medications) are prescribed to prevent new clot formation. Depending on the extent of the disease and the condition of the blocked artery, surgical interventions such as bypass surgery may be planned if necessary (for example, if a leg artery is completely blocked, bypass surgery can be performed using a healthy vessel to create an alternative route).
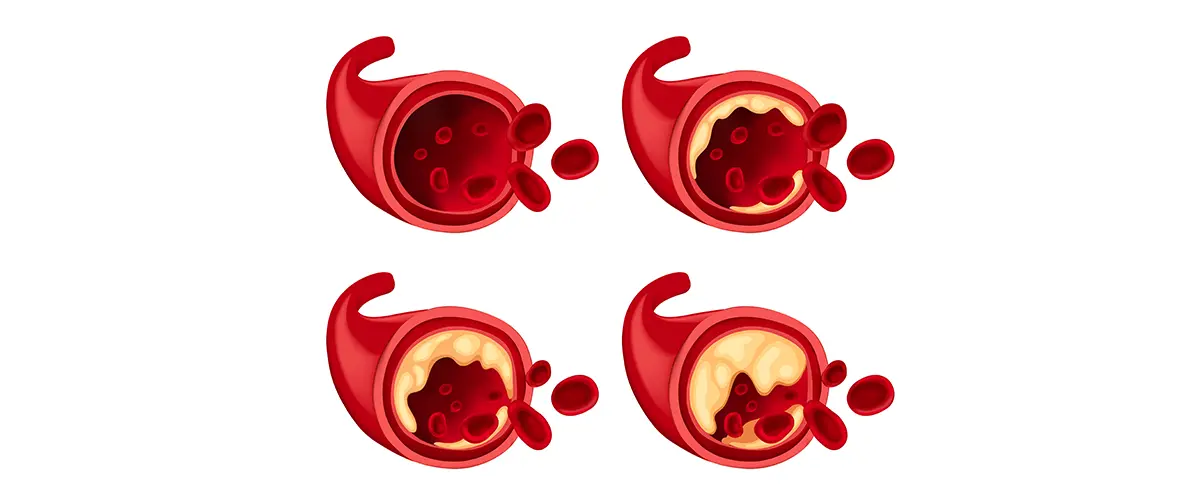
Peripheral Artery Disease (Leg Arterial Disease)
Peripheral artery disease is a circulatory disorder that occurs when there is narrowing or blockage in arteries outside the heart—especially in the arteries that supply the legs. The most common cause is atherosclerosis, which results from the buildup of fatty plaques in the artery walls. For this reason, peripheral artery disease usually appears in older adults and is more common in people with risk factors such as smoking, diabetes, high cholesterol, and high blood pressure. When the arteries in the legs become narrowed, the muscles do not receive enough blood, leading to symptoms such as pain and cramping, especially while walking. As the disease progresses, serious circulation problems in the legs may develop, such as non-healing wounds and tissue death.
Symptoms
The symptoms of peripheral artery disease develop gradually and become more severe as the degree of arterial blockage increases:
Leg pain (claudication): The most common symptom is pain or cramping in the calf that occurs with walking and disappears with rest. After resting, the pain goes away, but as the narrowing worsens, pain can start to occur over shorter distances.
Rest pain: In advanced stages of the disease, pain may be felt in the feet or legs even while at rest (especially at night while lying down). This indicates that arterial blockage has reached a critical level.
Coldness and color changes: There may be a persistent feeling of cold, coldness in the legs and feet, and pallor or bluish discoloration of the skin. Pulses at the ankle and the top of the foot may be weak or not detectable.
Skin and nail changes: The skin becomes thinner, hair on the legs may fall out, and toenails may thicken and appear unhealthy.
Wounds and gangrene: Small wounds on the feet heal slowly or may not heal at all. In advanced stages, when blood flow is severely reduced, these wounds can deepen into ulcers or lead to gangrene (tissue death) in the affected area.
Diagnosis
The following methods are used to diagnose peripheral artery disease:
Physical examination: Pulses in the legs (e.g., groin, behind the knee, ankle pulses) are checked. Weak or absent pulses may indicate narrowing of the corresponding artery. Changes in skin color and temperature of the legs are also evaluated.
Ankle-brachial index (ABI): Using a special device, blood pressure at the ankle is compared to blood pressure in the arm. Normally, these values are similar; if there is narrowing in the leg arteries, the ankle pressure will be lower. This simple test is useful for detecting peripheral artery disease.
Doppler ultrasound: With vascular ultrasound, blood flow in the leg arteries is visualized. This method measures the flow rate and degree of blockage inside the arteries, pinpointing the location of narrowing. Color Doppler ultrasound is a non-invasive and easy diagnostic method.
Angiographic imaging: For definitive diagnosis and treatment planning, angiography may be performed. Magnetic resonance angiography (MRA) or computed tomography angiography provides a detailed view of the leg arteries. If necessary, conventional (catheter-based) angiography is also used to determine the exact location and extent of the blockage.
Treatment
Lifestyle modifications: The most important step in peripheral artery disease is quitting smoking. Additionally, regular exercise (e.g., walking programs), healthy and low-calorie eating, and weight management can slow the progression of the disease. These measures also help slow the process of atherosclerosis, benefiting the entire vascular system.
Medication: Doctors may prescribe various medications to improve circulation and prevent clot formation. For example, vasodilators to increase blood flow, pain-relieving medications, or blood thinners (such as aspirin) may be used. Additionally, if cholesterol and blood pressure are elevated, medication to manage these conditions will be prescribed.
Endovascular treatments: In cases where symptoms are significantly increasing or the artery is severely narrowed, interventional treatments such as angioplasty and stent placement may be considered. In this procedure, during angiography, a balloon catheter is used to expand the narrowed area, and a stent is placed to keep the artery open. This procedure is typically performed through the groin and allows the patient to return to normal life in a short period.
Surgical treatment (bypass): If the blockage in the artery is very advanced or covers a long segment, bypass surgery may be required. In this surgery, a healthy vessel from another part of the body (usually a leg vein, saphenous vein) or an artificial graft is used to create a new path beyond the blockage. This allows blood to be redirected around the blocked area, restoring circulation in the leg.
Treatment of developing complications: For advanced peripheral artery disease, wound care and the removal of dead tissue (debridement) may be necessary. If gangrene has developed, amputation of the affected part (such as a finger or limb) may be required to prevent the spread of infection. This is considered a last resort and is usually avoided with early diagnosis and treatment.
Carotid Artery Disease (Carotid Artery Stenosis)
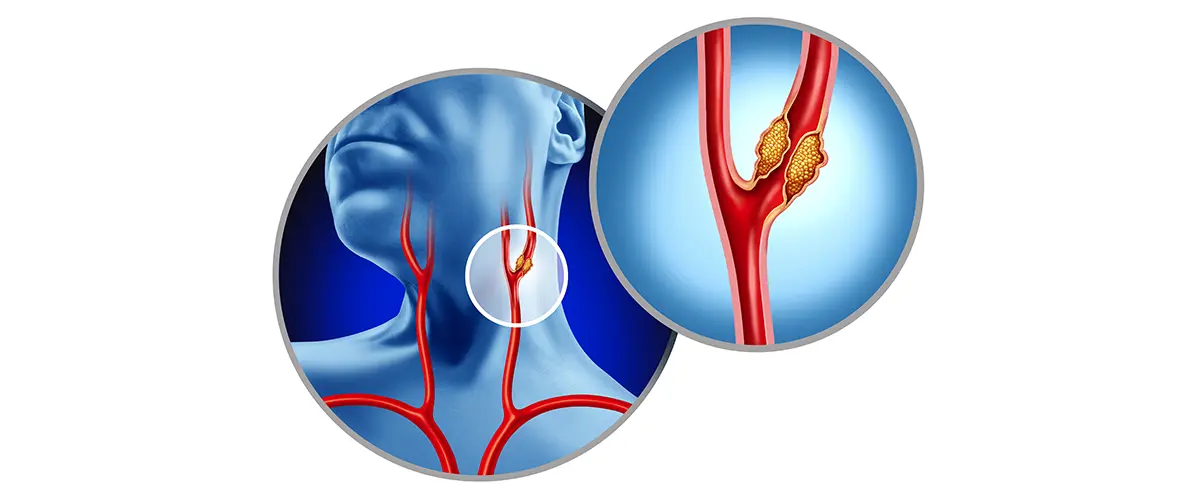
Carotid artery disease is the narrowing and blockage of the carotid arteries, located on both sides of the neck, due to the buildup of atherosclerotic plaques. Since the carotid arteries supply blood to the brain, significant narrowing or blockage in these arteries reduces blood flow to the brain, increasing the risk of stroke. The most common cause is atherosclerosis; risk factors such as high cholesterol, high blood pressure, smoking, diabetes, and advanced age play a role in the development of the disease. As these risks increase, the likelihood of developing carotid artery disease also rises. Carotid artery narrowing typically progresses slowly and may not show symptoms initially. However, clinical signs appear when the narrowing reaches a critical level or when a clot forms in the affected artery and is carried to the brain, potentially causing a stroke.
Symptoms
The symptoms of carotid artery disease are caused by temporary or permanent disruption in blood circulation to the brain. Common symptoms include:
Sudden numbness, tingling, or weakness on one side of the body, including the face, arm, or leg (usually a sign of stroke or a transient ischemic attack).
Speech difficulties or trouble understanding speech (medically known as aphasia).
Vision loss: Sudden temporary vision loss or blurred vision in one or both eyes.
Headache and dizziness: Sudden, severe headache; unexplained dizziness and balance problems. These symptoms are sometimes overlooked by patients but can be a warning sign of a stroke.
Note: If carotid artery narrowing is mild, it may not cause any symptoms. Symptoms are usually noticed when temporary brain circulation disturbances (transient ischemic attacks) or a stroke occur.
Diagnosis
Physical examination: The carotid arteries are listened to with a stethoscope to detect abnormal sounds called bruits. If there is narrowing in the carotid artery, a bruit may be heard in the neck due to turbulence in blood flow.
Doppler Ultrasound (Carotid Ultrasound): This is the first choice for diagnosing carotid artery disease. The ultrasound visualizes the plaques inside the artery and measures the percentage of narrowing. This method is non-invasive (does not require intervention) and does not cause discomfort to the patient.
Magnetic Resonance Angiography (MRA) / Computed Tomography Angiography (CTA): MRA or CTA can be used to create detailed maps of the neck arteries. These imaging techniques show the location and severity of the narrowing in three dimensions and assess the blood supply to the brain tissue.
Conventional angiography: For definitive diagnosis and treatment planning, catheter angiography may be performed through an artery in the groin. In this invasive method, contrast dye is injected into the carotid artery to obtain detailed images. If necessary, during the angiography procedure, a stent may be placed in the narrowed area for treatment.
Treatment
Medical (conservative) treatment: If carotid artery narrowing is mild or moderate and asymptomatic, the primary approach is medication and management of risk factors. Cholesterol-lowering statins, blood pressure and diabetes medications are used to slow the process of atherosclerosis. Blood thinners (e.g., aspirin) are used to prevent clot formation in the artery. This approach aims to reduce the risk of stroke.
Surgical treatment – Carotid endarterectomy: The classic surgical treatment for carotid artery stenosis is endarterectomy. In this surgery, the narrowed carotid artery in the neck is opened, and the plaque attached to the inner surface of the artery is surgically removed. The procedure is typically performed under local or general anesthesia, and after the plaque is removed, the artery wall is repaired and closed. Carotid endarterectomy is an effective method for significantly reducing the risk of stroke in suitable patients.
Endovascular treatment – Stenting: In some patients, carotid stenting is an alternative to surgery. In this method, a catheter is inserted through the groin to reach the narrowed area, and a metal tube called a stent is placed in the narrowed segment. The stent expands the artery from the inside, supporting the artery wall and restoring blood flow. Endovascular stenting is recommended only for appropriate cases and for patients who are not suitable candidates for surgery due to their general condition.
Follow-up and lifestyle: It is crucial for everyone with carotid artery disease to manage risk factors. Quitting smoking, healthy eating, regular exercise, and bringing blood pressure and cholesterol levels into the ideal range slow the progression of existing narrowing and reduce the risk of new vascular problems. After surgery or stenting, patients are monitored regularly through follow-up visits, including ultrasound and physical exams.
Note: The choice of treatment method depends on the degree of stenosis, the patient’s general health condition, and surgical risk. Both surgery and stent placement, when performed at experienced centers, significantly reduce the risk of stroke and can achieve similar success.
Aneurysm (Vascular Ballooning)
An aneurysm is a condition where a weakness in the wall of an artery causes the affected area to balloon or dilate. This is why it is also commonly referred to as a vascular balloon. Aneurysms can develop in any artery in the body, but they are most commonly seen in the body’s largest artery, the aorta (especially in the abdominal aorta), or in the brain arteries. As the weakened arterial wall continues to expand, the aneurysm grows, and the risk of rupture increases. If an aneurysm ruptures, it leads to uncontrolled internal bleeding, which requires urgent intervention and poses a life-threatening situation. High blood pressure, atherosclerosis, smoking, genetic predisposition, connective tissue diseases that weaken the artery walls, and trauma can all contribute to the development of an aneurysm. Abdominal aortic aneurysms are particularly more common in men and individuals over the age of 65.
Symptoms
The symptoms of an aneurysm vary depending on the artery it affects and its size:
No symptoms: Small aneurysms usually do not show any symptoms. For example, a small abdominal aortic aneurysm might be detected accidentally during an ultrasound for another reason, and the patient may not be aware of it.
Brain aneurysm symptoms: If an aneurysm in the brain grows and exerts pressure on surrounding tissues, it may cause symptoms such as headaches, vision disturbances (e.g., double vision), or drooping of the eyelid. If the brain aneurysm ruptures, it leads to sudden and severe headaches (described by patients as “the worst headache of my life”), nausea, vomiting, stiff neck, light sensitivity, loss of consciousness, and potential paralysis. These are signs of a subarachnoid hemorrhage (bleeding under the brain’s membranes) and require urgent medical intervention.
Abdominal aortic aneurysm symptoms: Aneurysms in the abdomen typically do not cause symptoms until they grow larger. A large abdominal aneurysm may cause a pulsating mass in the abdomen (felt like a pulse), and persistent pain in the abdomen or lower back. If the aneurysm ruptures, sudden severe abdominal and back pain, low blood pressure, fainting, and shock symptoms can occur. This situation is life-threatening and requires emergency surgical intervention.
Diagnosis
Imaging methods: Aneurysms are mostly diagnosed through imaging techniques. Many aneurysms are detected incidentally during examinations for other conditions. Ultrasonography is a commonly used, fast, and non-invasive method for screening and monitoring abdominal aortic aneurysms. The diameter of the aneurysm is measured during ultrasound to track if it has grown.
Computed Tomography (CT) / Magnetic Resonance (MR): CT or MR imaging is used to assess the location and size of the aneurysm in detail. Particularly for brain aneurysms, CT angiography or MR angiography is used to visualize the brain vessels and detect the presence of ballooning. These methods also show the relationship of the aneurysm with surrounding structures and any signs of rupture.
Conventional angiography: For both aortic and brain aneurysms, catheter angiography provides invaluable information for diagnosis and treatment planning. Contrast dye is injected into the artery through the femoral artery, allowing precise visualization of the aneurysm’s location, shape, and its effects on surrounding vessels. For brain aneurysms, lumbar puncture (spinal tap) can also be used, especially when there is suspicion of bleeding, to check for blood in the cerebrospinal fluid.
Treatment
Aneurysm treatment is planned based on its size, location, and the risk of rupture. For small and asymptomatic aneurysms, doctors typically recommend regular follow-up. Imaging is performed at regular intervals to monitor the growth rate of the aneurysm. Managing risk factors (e.g., lowering blood pressure, quitting smoking) can also help slow its growth.
Open surgical treatment: For large or high-risk aneurysms, open surgery may be preferred. For example, in abdominal aortic aneurysms, the abdominal area is opened, and the aneurysmal sac is removed, replacing it with a synthetic graft. This replaces the weakened section of the artery with a healthy graft. Open surgery, especially in younger and generally healthy patients, can provide a long-term, permanent solution.
Endovascular (minimally invasive) treatment: Today, many aneurysms can be treated without the need for surgical cuts, using a catheter that is inserted into the artery. In this method, a catheter is passed through the femoral artery, and a stent-graft is placed at the aneurysm site (a procedure known as EVAR, commonly used for aortic aneurysms). For brain aneurysms, coils made of fine platinum wire are used to fill the aneurysmal sac. Endovascular methods offer shorter hospital stays, faster recovery times, and generally lower complication risks compared to open surgery.
Emergency treatment: In cases of ruptured aneurysms (e.g., a bleeding brain aneurysm or a ruptured aortic aneurysm), emergency treatment is essential. Once the patient is stabilized, surgery or endovascular procedures are performed as soon as possible to seal the aneurysm and prevent further bleeding. For brain hemorrhage, the aneurysm may need to be clipped or filled with coils within a few days. Early intervention is critical in reducing life-threatening risks.
Conclusion

In summary, arterial diseases – including atherosclerosis, arterial blockages, peripheral artery disease, carotid artery disease, and aneurysms – are serious health problems that can lead to significant complications but are largely preventable or treatable. Adopting healthy lifestyle habits is essential to prevent these conditions. Not smoking, eating a healthy diet, exercising regularly, controlling body weight, and managing risk factors such as blood pressure and cholesterol help keep arteries healthy. It is particularly important for those with a family history of vascular diseases or risk factors such as diabetes to undergo regular check-ups with their doctor for early diagnosis.
If you notice any symptoms of arterial disease (e.g., chest or leg pain with exertion, weakness on one side of the body, speech problems, sudden vision loss), do not hesitate to seek medical attention. Remember, this article is for informational purposes only; medical advice is required for a definitive diagnosis and treatment. By adopting a healthy lifestyle and paying attention to your body’s warning signs, you can significantly reduce the risk of arterial blockages and similar vascular diseases. This will increase your chances of living a longer, healthier, and higher-quality life.
Arterial Blockages and Peripheral Diseases - FAQ
How to Recognize Circulatory Problems?
If you experience symptoms such as leg pain, coldness, color changes, or cramping pain while walking (claudication), it could be a sign of arterial blockage or insufficiency.
What is Peripheral Artery Disease (PAD)?
What is Arterial Bypass?
Arterial bypass surgery involves rerouting blood flow around a blocked or narrowed segment of an artery using a vein taken from the body or a synthetic graft. It is most commonly performed on the arteries in the legs.
When is Arterial Bypass Necessary?
Severe pain in the leg while walking (claudication)
Rest pain due to advanced arterial blockage
Tissue loss, gangrene, or non-healing wounds
Situations where interventional procedures (angioplasty, balloon) are insufficient
Which Vessels are Used for Bypass?
Saphenous vein: Taken from the inner side of the leg, it is the most commonly used natural graft.
Arm vessels (basilic, cephalic veins).
If suitable vessels are not available, synthetic grafts (PTFE, Dacron) may be used.
Is bypass surgery an open procedure, and is it risky?
Yes, it is an open surgery. However, when performed by experienced hands, the success rate is high. Risks include bleeding, infection, graft blockage, and wound problems. Smoking and uncontrolled diabetes increase the risk.
How long does it take to recover after bypass surgery?
The hospital stay usually lasts between 3 to 7 days. Wound healing can take 2 to 4 weeks. Walking comfort improves significantly after a few weeks. The complete recovery time varies from patient to patient.
What should be observed after arterial bypass surgery?
Regular use of blood thinners
Complete cessation of smoking
Monitoring of the wound and dressing changes
Follow-up with vascular ultrasound or Doppler to check graft patency
Controlled exercise program
Do herbal or natural supplements help improve circulation?
Some herbal products (such as ginkgo biloba, gotu kola, grape seed extract) can, to a limited extent, support circulation. However, they should not be used without a doctor’s recommendation, as some of these may interact with blood thinners.
What is Botox and how does it work?
Botulinum toxin (Botox) is a substance that temporarily blocks nerve-muscle communication, preventing muscle contraction. Due to this effect, it is used for both aesthetic and medical purposes.
In which situations is Botox applied?
Botox is used for treating wrinkles, excessive sweating (hyperhidrosis), migraines, teeth grinding (bruxism), and neck spasms, among many other conditions.
What is sweating Botox?
Sweating Botox is applied to areas with excessive sweating, such as the palms, armpits, and soles of the feet. Botox temporarily blocks sweat glands, and its effect can last for 6 to 8 months.
How does Botox work in migraine treatment?
Botox, when applied to certain muscle groups, reduces the release of substances that transmit pain signals from nerve endings. In chronic migraine patients, it can help decrease the frequency and intensity of attacks.
When can one return to daily activities after Botox?
After the procedure, the person can immediately return to normal activities. However, activities such as sports, massage, and sauna should be avoided for 24 hours.
Is Botox permanent?
No, Botox’s effect is temporary and typically decreases over 4-6 months. With regular applications, the duration of its effects may be extended.
Is there a relationship between stress and vascular diseases?
Yes, chronic stress increases cortisol and adrenaline levels, which can contribute to arterial narrowing. It also leads to secondary harmful behaviors such as poor sleep, poor nutrition, and smoking. Stress management is a supportive approach for all vascular diseases.
How is peripheral angiography performed?
A thin plastic catheter is inserted into the artery from the groin or wrist, and an X-ray sensitive contrast material is injected to visualize the vascular structure. The procedure typically lasts about 20-30 minutes under local anesthesia.
What is balloon angioplasty?
Balloon angioplasty involves placing a special balloon at the blocked area, which is inflated in a controlled manner to widen the artery. In most patients, a stent is also placed during the same procedure.
When is a peripheral stent needed?
A stent is preferred when sufficient opening cannot be achieved with balloon angioplasty, when there is a high risk of elastic recoil, or in long lesions. Nitinol (flexible) stents are commonly used in leg arteries.
What should I pay attention to after angiography?
The catheter entry site (groin/wrist) should be kept clean and dry for 24 hours. Avoid heavy lifting and exercise for 3-5 days. It is critical to use blood thinners and cholesterol medications as prescribed by your doctor.
Can deep vein thrombosis (DVT) be treated with angiography?
In acute ilio-femoral DVT, catheter lysis (using thrombolytic drugs) or mechanical thrombectomy can be applied to dissolve the clot; balloon and stenting may be required afterward. Proper patient selection is crucial.
What are the main risks of peripheral angiography?
The main risks include bleeding/hematoma at the site of the vessel puncture, contrast nephropathy, allergic reactions, and rarely, vessel rupture or the formation of an acute clot. With an experienced team and modern equipment, these risks are minimized.
What medications are used in the treatment of arterial blockage?
Main drug groups used in arteriosclerosis:
Blood thinners (Aspirin, clopidogrel, etc.)
Cholesterol reducers (statin group)
Vasodilator agents (like cilostazol)
Blood pressure and diabetes medications (in case of accompanying conditions)
These drugs aim not to open the artery, but to stabilize the current condition and prevent new events.
Which foods should I avoid to reduce the risk of arteriosclerosis?
Processed foods containing trans fats
Excessive salt and refined sugar
Fried foods and margarine
Fast food and ready-made sauces
Excessive consumption of red meat and offal
What is EVAR/TEVAR?
Endovascular aneurysm repair (EVAR: abdominal; TEVAR: thoracic aneurysm) is an internal repair of the artery using occlusive stent-graft systems. Compared to open surgery, it offers less blood loss and a shorter recovery time.
What is a permanent tunneled catheter, and what is it used for?
Permanent tunneled catheters (such as Hickman, Permcath) are special catheters used in patients who require long-term venous access, which reduce the risk of infection. They are typically preferred in situations such as hemodialysis, chemotherapy, and long-term antibiotic treatment.
What is a port catheter?
A port catheter is a small reservoir fully implanted under the skin. Medication is delivered through it using a special needle. It is used in patients who require chemotherapy or long-term venous access. It is a long-term, comfortable, and cosmetic solution.
What is the difference between a temporary catheter and a permanent catheter?
Temporary catheters (e.g., subclavian, jugular, femoral) are used for short periods and are generally located on the skin surface. Permanent catheters, on the other hand, have a tunneled structure designed for longer-term use, reducing the risk of infection.
Is inserting a port or tunneled catheter painful?
No. It is usually performed under local anesthesia and mild sedation. There may be slight pain after the procedure, but it typically resolves within a few days.
What should be considered after catheter insertion?
The insertion site should be kept clean and dry.
Regular dressing and medical check-ups are necessary.
Bathing can be done if the port needle is not inserted.
If there are signs of infection such as fever, redness, or discharge, immediate medical attention should be sought.
How long can a port or tunneled catheter be used?
With proper care, port catheters can be used for 2–5 years, and tunneled catheters can be used for months or even years. They do not need to be removed unless there is an infection, blockage, or mechanical issue.
What is contrast nephropathy, and do I have a risk?
Contrast agents can temporarily impair kidney function. Diabetes, advanced age, high creatinine levels, or dehydration increase the risk; however, this risk can be reduced by adequate fluid intake before and after the procedure, and, if necessary, protective serum treatment.
Which arterial blockages require surgery?
Arterial blockages that cannot be cleared with medication or interventional methods, or those causing serious walking impairments or tissue loss risk, are opened surgically.
How can I make an appointment?
You can quickly reach us via WhatsApp using the “Randevu Al” button on our website or by filling out the contact form.