Veins are the vessels that carry dirty blood from our body back to our heart. These vessels have valves that work in one direction. The valves that open when the muscles move, close when they relax, preventing the blood from flowing back despite gravity. However, these valves can be damaged in diseases that affect the venous system, causing the blood to flow back and accumulate in the veins. As a result, various problems such as burning and aching pain in the legs, swelling, darkening of the skin color, widening of the veins and taking a tortuous shape, or formation of clots inside the veins can occur. Vein diseases are encountered in a wide range of situations, from simple cosmetic problems (capillary varicose veins) to life-threatening conditions (such as deep vein thrombosis).
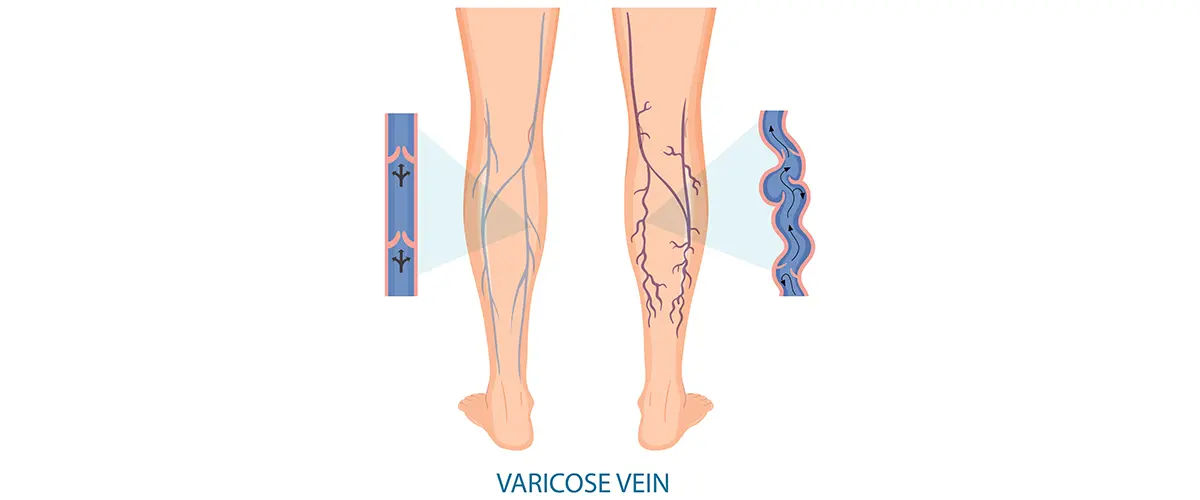
Varicose Veins and Capillary Dilations
Varicose veins are bluish-green, twisted veins that become visible under the skin as a result of abnormal expansion and elongation of the veins. They occur especially in the legs and often cause pain, heaviness and a burning sensation. Swelling in the ankles in the evening, night cramps, itching and restlessness are also among the symptoms of varicose veins. Finer capillary dilations create a red-purple spider web appearance on the skin and are usually a cause for cosmetic concern. Varicose veins are quite common; varicose veins are seen in roughly one-third of the population. The weakening of the vein wall and valve damage play a role in the formation of varicose veins.
Risk factors for varicose veins
The following factors increase the risk of developing varicose veins:
- Genetic predisposition: Having a family history of vein disease (e.g. varicose veins)
- Gender: More common in women
- Pregnancy: Pregnancy (increased pressure and hormonal effects)
- Obesity: Being overweight
- Position: Having to stand or sit still for long periods
Varicose veins usually follow a progressive course. This disease, which has 6 stages, has a wide range from stage 1, where there are only complaints without any visible veins, to stage 5, where the brown skin color changes on the legs and open wounds form. Over time, the vicious cycle begins as the veins become more visible, the valves in the veins deteriorate, and vascular leakage occurs. If left untreated, complications such as superficial thrombophlebitis or venous ulcer may develop. Fortunately, today there are very effective methods for the treatment of varicose veins. Sclerotherapy (vein drying with medication), laser and radiofrequency ablation non-surgical techniques or, in advanced cases, surgical methods can be used to treat varicose veins. Thus, pain and cosmetic complaints are eliminated and quality of life is improved.
Chronic Venous Insufficiency
Chronic venous insufficiency (vein insufficiency) is the condition in which blood leaks back and pools in the leg veins as a result of the valves in the leg veins losing their function. As a result of this chronic condition, there is constant swelling in the legs, increased pressure in the veins, dark pigmentation on the skin (brown spots) and hardening under the skin over time. Patients usually complain of pain, fullness and fatigue in their legs. Skin changes (dryness, itching, eczema-like rashes) indicate that chronic venous insufficiency is progressing. In advanced stages, wounds that are difficult to heal (venous ulcers) may occur around the ankle.
Chronic venous insufficiency is usually seen in those with advanced varicose vein disease or after a deep vein thrombosis (post-thrombotic syndrome). Therefore, it is important to treat existing varicose veins and to take regular check-ups and precautions in patients who have had DVT. The first step in treatment is to use compression stockings, elevate the legs during the day and exercise. The effects of venous insufficiency can be reduced with interventions (laser, surgery, etc.) targeting the underlying varicose veins. By controlling chronic venous insufficiency with treatment and follow-up, swelling and skin problems in the patients’ legs can be improved and new ulcer formation can be prevented.
Deep Vein Thrombosis (DVT)
Deep vein thrombosis (DVT) is the formation of a blood clot in the deep veins (usually in the legs, sometimes in the arms). This clot can partially or completely block the vein, causing symptoms such as pain, tenderness, increased heat and swelling in the leg.
Although DVT is not always fatal on its own, its greatest danger is when the clot breaks away from the vein wall and is carried to the lungs through the bloodstream. Pulmonary embolism, which occurs when a clot blocks the pulmonary arteries, is a life-threatening emergency that causes sudden shortness of breath and chest pain.
Certain risk factors play a role in the development of DVT: Factors such as prolonged immobilization (e.g. long flights or bed rest after surgery), major surgeries, leg casts, pregnancy, birth control pills or hormone treatments, blood clotting disorders and smoking increase the risk of DVT. When DVT is suspected, it is necessary to see a doctor without delay. Diagnosis is usually made with a Doppler ultrasound. In treatment, blood thinners (anticoagulant) are used to prevent the clot from growing and reaching the lungs. In necessary cases, hospitalization and advanced treatments (such as clot-dissolving drugs or filter placement) may be applied. It is important for patients who have had DVT to use compression stockings in the long term and to have regular physician follow-ups to prevent post-thrombotic syndrome and new clot formation. In some patients, genetic testing may be necessary to evaluate the tendency to clot.
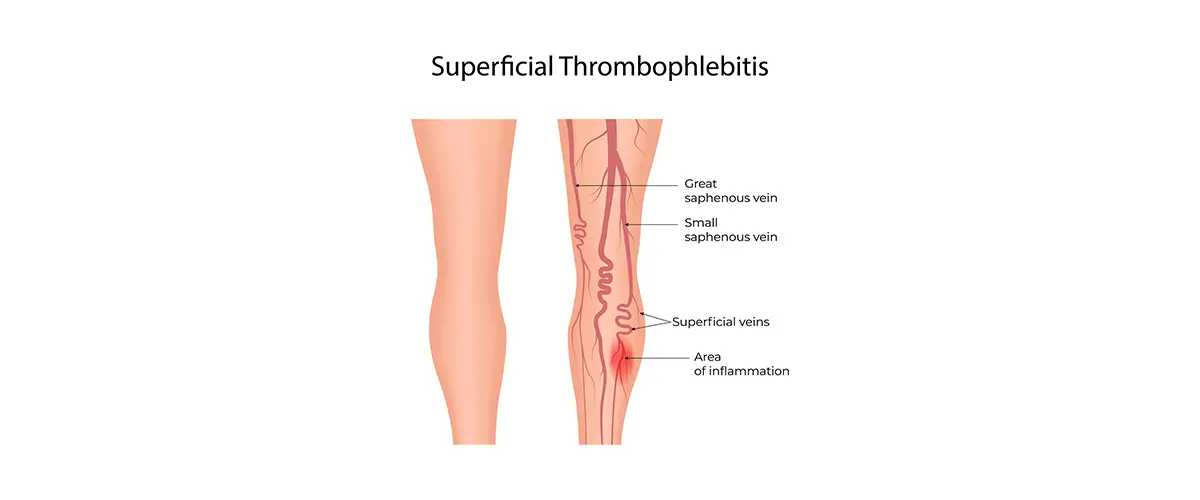
Superficial Thrombophlebitis
Superficial thrombophlebitis is the formation of a clot in a superficial vein close to the skin, causing inflammation of the vein. It usually occurs in varicose (previously dilated) superficial veins. The affected area is characterized by redness of the skin, localized warmth, and swelling and tenderness in the vein in the form of a hard band that can be felt. Superficial thrombophlebitis is a milder condition that tends to heal on its own in most cases; unless it has spread to the deep vein system, the probability of a clot reaching the lungs is low. However, it is still important to be evaluated appropriately, because in some cases, superficial thrombophlebitis can progress to deep vein thrombosis.
Superficial thrombophlebitis is usually treated with resting the affected area, warm compresses, and anti-inflammatory painkillers (NSAIDs). If the clot is very widespread or close to the deep vein system, doctors may also recommend short-term blood thinning therapy. Since thrombophlebitis attacks may recur in people with underlying varicose veins, treatment of varicose veins (laser, sclerotherapy, etc.) is recommended to prevent recurrence of this problem in the long term. Superficial thrombophlebitis usually resolves within a few weeks with the right approach and does not leave any permanent damage.
Venous Ulcer (Varicose Vein)
Venous ulcers are one of the most advanced stages of venous diseases. They are skin wounds that usually occur on the inside of the legs, especially above the ankle, and usually have dark skin color changes. These wounds occur as a result of damage to the skin due to high pressure and circulatory disorders in the veins. Since the skin’s blood and oxygen supply is disrupted as a result of chronic venous insufficiency, a small bump or cut can easily turn into a deep wound. Venous ulcers are wounds that are difficult to heal; sometimes they can remain open for months and even if they heal, they tend to recur. Problems such as discharge from the wound, bad odor and risk of infection seriously reduce the quality of life of patients.
The rate of developing venous leg ulcers in patients with varicose veins is approximately 1%, and this rate increases with age. The most important cause of venous ulcers is long-term varicose disease and venous insufficiency. These wounds usually occur on the basis of skin hardening and dark skin changes called lipodermatosclerosis. The main goal in treatment is to reduce venous hypertension, which causes the wound. The pressure in the leg veins is reduced by using pressure bandages or varicose stockings; regular wound care is used to control infection and ensure wound closure. In addition, treating varicose veins with methods such as laser and radiofrequency and eliminating leaks in superficial veins are important parts of venous ulcer treatment. In order to prevent these wounds, many of which can heal with appropriate treatment, from recurring after they have healed, patients should have varicose vein treatments and wear varicose stockings for the recommended period.
Conclusion
Thanks to the advances in modern medicine, vein diseases can now be treated effectively. Diseases such as varicose veins, chronic venous insufficiency, thrombosis, thrombophlebitis and venous ulcers are much easier to control when diagnosed early. If you notice swelling, pain, visible veins or non-healing wounds in your legs, do not ignore them. Remember, even a small varicose vein problem can turn into a serious problem over time. Take care of your vein health for a healthy life and a comfortable future.
In our clinic, the diagnosis and treatment of vein diseases are performed by expert cardiovascular surgeons with up-to-date and innovative methods. If you have symptoms or think you are at risk, you can make an appointment without delay and undergo a specialist evaluation. Early precautions can prevent major problems in the future. Contact us today – take the first step towards healthy and pain-free legs!
Varicose Vein Treatment - FAQ
What are varicose veins and how do they occur?
Varicose veins occur as a result of the dysfunction of the valves in the veins, causing blood to flow backward and the veins to enlarge. Genetic predisposition, prolonged standing, pregnancy, and obesity are factors that increase the risk.
Is varicose vein treatment with laser painful?
No. Endovenous laser treatment is performed under local anesthesia and is generally painless. The patient is usually discharged on the same day.
When is an IVC (inferior vena cava) filter placed?
An IVC filter is placed when the risk of pulmonary embolism is high but the patient cannot use or is using anticoagulant medication. The filter is placed temporarily or permanently to prevent clots from traveling to the lungs.
What is sclerotherapy?
Sclerotherapy is a minimal invasive treatment method where a sclerosing substance (irritating medication) is injected into varicose veins to close the veins and cause them to disappear over time. It can be applied in liquid or foam form.
What is the difference between foam sclerotherapy and liquid sclerotherapy?
In foam sclerotherapy, the medication is mixed with air to increase its density, making it more effective for larger and superficial varicose veins. Liquid sclerotherapy, on the other hand, is suitable for finer veins.
Is sclerotherapy a painful procedure?
No. The procedure is generally painless or causes minimal discomfort because it is done with very fine needles. Local anesthesia is not required. The duration of the procedure is 15–30 minutes.
What precautions should be taken after sclerotherapy?
Compression stockings should be worn after the procedure.
Heavy exercise should be avoided for 24 hours.
Sun exposure and hot baths are not recommended.
Light walking is encouraged during the first week.
Does sclerotherapy provide a permanent solution?
The treated veins will not return; however, if the person is predisposed to developing varicose veins, new veins may develop over time. Regular follow-up and lifestyle changes are recommended.
Who is sclerotherapy not suitable for?
Individuals with active DVT (deep vein thrombosis).
Pregnant women.
Those with an allergy to sclerosing agents.
Patients with severe arterial circulation disorders.
In these cases, alternative treatment options should be considered.
Which medications are used in the treatment of varicose veins?
Medications that increase venous tone and support microcirculation are used in the treatment of varicose veins. The most commonly preferred ones are:
Diosmin + Hesperidin combinations
Rutoside and similar flavonoids
Horse chestnut extract (escin)
These medications do not stop the progression of varicose veins but can alleviate symptoms.
What is personalized varicose vein treatment?
Personalized varicose vein treatment is planned based on the patient’s vein structure, lifestyle, and aesthetic expectations, using a combination of techniques such as laser, foam, sclerotherapy, and miniflebectomy. The approach follows the idea that “one method does not fit all,” and an individualized algorithm is prepared.
Are these medications enough on their own?
No. Medications for varicose veins, vascular blockage, and wound care are supportive treatments. Physical therapy, lifestyle changes, and surgery or minimally invasive procedures should be combined.
How is a personalized treatment plan created?
The treatment plan is generally determined based on color Doppler ultrasound, clinical findings, and the patient’s expectations. Different types of structures, such as superficial varicose veins, reticular veins, saphenous veins, or perforator insufficiency, require different methods.
What is the CLACS method?
CLACS (Cryo-Laser & Cryo-Sclerotherapy) is a modern technique that combines laser therapy and sclerotherapy with ultra-fine needles, under the accompaniment of cold air (cryo). It is particularly used for the treatment of fine saphenous veins and for aesthetic purposes.
Who is CLACS suitable for?
CLACS is ideal for individuals who are bothered by the appearance of fine purple/red veins on their legs but do not have large varicose veins. It is applied by considering skin type, vein thickness, and color mapping.
Is CLACS painful?
No. Thanks to the application of cold air, pain is minimal. Aside from the sensation of the needle insertion, no significant discomfort occurs. Sessions generally last for a short time.
What precautions should be taken after CLACS?
Protect from sunlight (especially for individuals with fair skin).
Use compression stockings (if necessary).
Avoid heavy exercise and hot environments like saunas for the first 24 hours.
Temporary redness and slight swelling on the vein are normal.
What natural foods increase blood flow?
Ginger, garlic, onion
Beetroot (with its nitric oxide boosting effect)
Dark leafy green vegetables (containing folic acid and nitrates)
Cocoa and dark chocolate (70% and above)
Turmeric (with anti-inflammatory properties)
Does nutrition replace medication treatment?
No. Nutrition is a supportive component of treatment but is not sufficient on its own. In cases such as vascular blockage, ulcerative wounds, or advanced varicose veins, medical or interventional treatments recommended by your doctor should be prioritized.
How does daily exercise affect vein health?
Exercise increases circulation, activates the calf muscle pump, and balances venous pressure. Brisk walking, cycling, water exercises, and exercises for varicose veins and vascular blockages are especially recommended.
How does smoking affect veins?
Smoking damages the vessel walls, increases clotting, and causes narrowing of the veins. It increases the risk of peripheral artery disease, chronic wounds, and amputations. It significantly reduces treatment success.
What should I pay attention to as someone who works on their feet?
Take a short walk or stretch every 30 minutes.
Take a cold water shower on your legs (increases venous tone).
Rest with your legs elevated for 15-20 minutes after work.
Use daily compression stockings.
What should I pay attention to as someone who works while sitting?
Get up every hour and walk for a few minutes.
Perform ankle exercises (up and down movements).
Place a 10–15 cm support under your feet to correct your leg position.
Avoid crossing your legs while sitting at the desk.
How should I eat for varicose veins and vascular health?
Vegetables and fruits rich in fiber.
Dark-colored foods containing antioxidants (blueberries, pomegranate, red grapes).
Omega-3 fatty acids (walnuts, flaxseeds, fish).
Limit salt and saturated fat intake.
Consume adequate water daily (at least 2 liters).
Does constipation worsen varicose veins, and what should I do?
Yes. Constipation increases intra-abdominal pressure, which strains the leg veins. Drinking plenty of water, eating high-fiber foods (whole grain products, vegetables, fruits), and maintaining regular physical activity can help prevent constipation and alleviate varicose veins.
What should I pay attention to for varicose veins and vascular health?
Avoid standing or sitting for long periods.
Rest with your legs elevated.
Use compression stockings regularly.
Do regular walking and exercises that engage the leg muscles, such as swimming.
How often should follow-up appointments be made after treatment?
After laser or foam varicose vein treatments, the first follow-up should be within the first week, then follow-ups are recommended again at 1 month and 3 months. For chronic wounds, weekly follow-ups are planned.
What is foam treatment and how is it applied?
Foam treatment involves injecting a special sclerosing agent into the varicose vein, causing the vein walls to stick together. The procedure is quick and is done while standing.
What is the difference between open surgery for varicose veins and laser treatment?
Open surgery involves removing the vein using traditional surgical methods. Laser treatment, on the other hand, is minimally invasive; it offers less pain, faster healing, and aesthetic advantages.
What is a compression stocking, and what does it do?
A compression stocking is a medical product that applies controlled pressure externally to the legs, helping to accelerate circulation and reduce swelling. It is commonly used in the treatment of varicose veins, venous insufficiency, DVT (deep vein thrombosis), and lymphedema.
Who needs compression stockings?
Compression stockings are recommended for patients with varicose veins, venous insufficiency, and lymphedema. They are also used for post-surgery swelling control. The appropriate pressure and size should be selected.
How are compression stockings classified (according to pressure levels)?
Compression stockings are generally classified between Class 1 and Class 4:
Class 1: Light varicose veins and preventive purpose (15–20 mmHg)
Class 2: Moderate varicose veins and swelling (20–30 mmHg)
Class 3: Severe venous insufficiency (30–40 mmHg)
Class 4: Lymphedema and severe swelling (over 40 mmHg)
How and when should compression stockings be worn?
Compression stockings should be worn immediately upon waking up, before any swelling occurs in the legs. The appropriate size should be selected with the help of a doctor or nurse. They should be removed while sleeping.
What is multi-layer compression bandaging?
Multi-layer compression bandaging is a treatment method that applies multiple layers of different materials (cotton dressing, short-long elastic bandages) to provide external, stable pressure and internal dynamic pressure. It is the gold standard for treating venous ulcers and lymphedema.
What is the difference between compression bandage and compression socks?
A bandage is used during the active treatment phase, while socks are typically used for maintenance therapy and prevention. The bandage provides more targeted and adjustable pressure, which offers an advantage in application.
Does compression therapy have side effects?
If applied improperly, it can lead to bruising, skin irritation, and circulation problems. Therefore, it must be measured and applied by a professional.